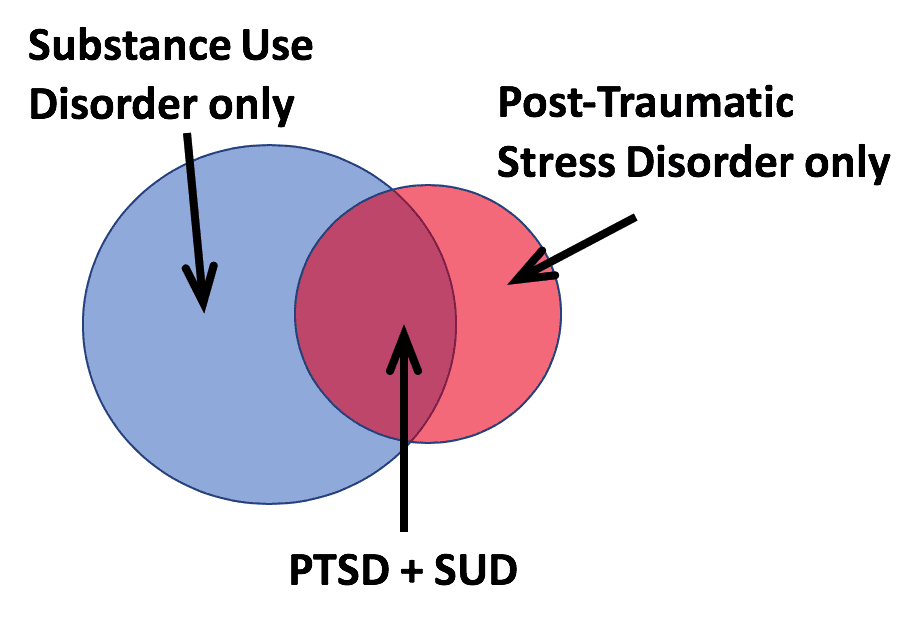
Most people who struggle with an addiction problem have also experienced significant past trauma. By the same token, 50-66% of individuals diagnosed with post-traumatic stress disorder (PTSD) also live with co-occurring addiction disorders. The presence of one or more mental health and substance use disorders (SUDs) in the same person is referred to as co-occurring disorders.
Co-occurring disorders can be difficult to diagnose because of overlapping symptoms. However, it is important to get the diagnoses right for integrated treatment of the whole person to take place. This is especially true when PTSD and SUDs co-occur together.
What is Post-Traumatic Stress Disorder?
- PTSD is a mental health disorder triggered by a terrifying event (either experienced or witnessed)
- It is normal for everyone who goes through a traumatic event to experience distress. PTSD is diagnosed if that distress lasts for months or years and interferes with daily functioning.
- Symptoms may include:
- Flashbacks or nightmares
- Severe anxiety
- Avoiding thinking or talking about the event
- Avoiding places, activities, or people that remind you of the event
- Negative thoughts about oneself or the world
- Hopelessness about the future
- Memory problems
- Difficulty with relationships
- Feeling emotionally numb
- Being easily startled or frightened
- Always being on guard
- Self-destructive behavior
- Difficulty concentrating or sleeping
- Irritability or anger outbursts
- Overwhelming guilt or shame
If you have problems with substances, chances are high that you have post-traumatic stress disorder, too (and vice versa!)
Substance abuse and post-traumatic stress disorder are both tragically common in our society and very often go hand in hand. According to current estimates, approximately 20 million American adults, 18 years or older, suffered from a substance use disorder over the past year. Meanwhile, over the same time period, approximately 8 million suffer from post-traumatic stress disorder. Of those who seek treatment for SUD, roughly half suffer from PTSD and of those with PTSD roughly half have an active SUD.
PTSD and SUD affect each other in important ways
- Studies show that there are genes that increase the risk of someone developing both PTSD and SUD.
- We know that certain life events and environments make both illnesses more likely.
- Having PTSD makes it much more likely that someone will develop an SUD and makes it harder to get successful treatment for SUD. This is sometimes referred to as the “self-medication hypothesis” – that people with PTSD sometimes abuse substances as a way to cope, or self-medicate, in the short term, even though substances make things much worse in the long run.
- Some studies have shown that having an SUD makes it more likely that an individual will be exposed to traumatic situations and, if this happens, to develop PTSD as a result.
The best treatments address PTSD and SUD together, rather than separately
Years ago, it was commonly taught that in order to treat PTSD, one had to first treat the substance use problems. It has also been suggested at times that to successfully treat a substance problem, one had to treat the PTSD first. Unfortunately, these myths continue in some places. However, research has shown clearly that the best treatment addresses PTSD and SUD simultaneously.
There are several evidence-based psychotherapeutic treatments that successfully address both SUD and PTSD. Seeking Safety (SS), Transcend, Integrated CBT (cognitive behavioral therapy), and Prolonged Exposure (PE) are some of the more widely known and researched approaches that have been shown to help with both disorders. In addition, several medications, including naltrexone (Vivitrol), disulfiram (Antabuse), topiramate (Topemax), and paroxetine (Paxil) have been shown to be components of successful treatment of the combined disorder. As with virtually all psychiatric illness, both psychotherapy and medication should be considered because for most individuals they work better together than separately.
Depending on the severity of symptoms, individuals suffering from SUD and PTSD may be treated through weekly outpatient visits, through outpatient visits more than once a week (often referred to as an Intensive Outpatient Program or IOP), in a residential rehabilitation facility, or on an inpatient psychiatric unit. While most people prefer the less intensive treatment setting, sometime a more intensive setting is needed in order to initiate appropriate interventions.
More research is urgently needed in this area
Given how common it is for someone with substance use disorder to also have PTSD, and vice versa, it is very important that we continue to learn more about how to treat these illnesses together, and not just separately. In the meantime, it is important for individuals to let their mental health providers know when they are experiencing symptoms of one or the other disorder and to seek treatment that takes both into consideration. PTSD and SUD both respond to good treatment and there are resources available to find providers in your area with the appropriate expertise.
If you or someone you know experiences mental health issues, it is important to seek help from a qualified professional. Our Resource Specialist can help you find expert mental health resources to recover in your community. Contact us now for more information on this free service to our users.
Author Bio: Andrew J. Gerber, MD, PhD, is the President and Medical Director of Silver Hill Hospital in New Canaan, Connecticut. His principal interests and research lie in studying the neurobiological bases of social cognition, particularly in relation to autism spectrum disorders and change in response to psychotherapy. He is a member of the American Academy of Child and Adolescent Psychiatry, American Psychiatric Association, and the American Psychoanalytic Association.
References
- Berenz, E.C., Coffey, S.F. (2012) Treatment of co-occurring posttraumatic stress disorder and substance use disorders, Curr Psychiatry Rep, 14(5): 469-477.
- Brady, K.T., Back, S.E., Coffey, S.F. (2004) Substance abuse and posttraumatic stress disorder, Curr Directions in Psychological Science, 13(5): 206-209.
- https://www.ptsd.va.gov/understand/common/common_adults.asp. Visited Sept 23, 2019.
- https://www.mayoclinic.org/diseases-conditions/post-traumatic-stress-disorder/symptoms-causes/syc-20355967. Visited Sept 23, 2019.
Photo by whoislimos on Unsplash
The opinions and views expressed in this guest blog do not necessarily reflect those of www.rtor.org or its sponsor, Laurel House, Inc. The author and www.rtor.org have no affiliations with any products or services mentioned in this article or linked to herein.
Recommended for You
- Co-occurring Disorders: The Link Between PTSD and Addiction - September 27, 2019