| Children & Teens |
| Black and Latinx children were about 14% less likely than White youth to receive treatment for their depression. (1) |
| Approximately 50% to 75% of youth in the juvenile justice system meet the criteria for a mental health disorder. (13) |
| Over 25% of Black youth exposed to violence have proven to be at high risk for post-traumatic stress disorder (PTSD). (1) |
| Approximately 10% of White and Hispanic adolescents engaged in alcohol use, compared to 7.3% for Black adolescents and 4.7% for Asian adolescents. (14) |
| In 2018, a study found that the suicide rate of Black children 5 to 12 was nearly twice that of White children of the same age. (6) |
| In 2022, suicide was the third leading cause of death for Black or African Americans, ages 15 to 24. In 2019, for Native Hawaiians/Pacific Islanders ages 15-24, suicide was the leading cause of death. (14) |
| Self-reported suicide attempts rose nearly 80% among Black adolescents from 1991 to 2019, while the prevalence of attempts did not change significantly among those of other races and ethnicities. (23) |
| Adolescents of color who identify as LGBTQ may be especially at risk of a suicide attempt. (23) |
| Black children and adolescents who died by suicide were more likely than White youths to have experienced a crisis during the two weeks before they died. (6) |
| Adults |
| Individuals identifying as being two or more races (24.9%) are most likely to report having a mental health disorder within the past year than any other race or ethnic group, followed by American Indian/Alaska Natives (22.7%), White (19%), and Black (16.8%) (4) |
| Black American adults are 20% more likely to experience serious mental health problems, such as major depressive disorder or generalized anxiety disorder. (2) |
| Although rates of depression are lower in Blacks (24.6%) and Hispanics (19.6%) than in Whites (34.7%), depression in Blacks and Hispanics is likely to be more disabling and persistent. (4) |
| In 2018, Asian Americans were 60% less likely and Hispanic Americans 50% less likely to have received mental health treatment than non-Hispanic Whites. (4) |
| American Indians/Alaskan Natives report higher post-traumatic stress disorder and alcohol dependence rates than any other ethnic or racial group. (20) |
| According to a 2019 study, African Americans have the highest lifetime prevalence of PTSD (8.7%) compared to their white (7.4%), Latino (7%) and Asian (4%) counterparts. (19) |
| Homelessness & Housing |
| Black Americans living below the federal poverty guidelines are 2x as likely to report serious psychological stress as those living 2x above the poverty level. (2) |
| The Black community comprises approximately 40% of the homeless population, 50% of the prison population, and 45% of children in the foster care system. (2) |
| Employment & Education |
| Psychiatric disorders in childhood have been linked to negative outcomes, including poor social mobility and reduced social capital. (3) |
| In the BIPOC community, childhood depression has been associated with increased welfare dependence and unemployment. (3) |
| Psychiatric and behavioral problems among BIPOC youth often result in school punishment or incarceration, but rarely mental health care. (15) |
| Incarceration & Mental Health |
| Students of color, students with disabilities and students that are impacted by trauma are disproportionately disciplined and arrested rather than receiving the support and services that allow them to remain in the classroom and continue to make educational progress. (17) |
| Students of color who drop out of school prematurely are more than right times more likely to end up in the criminal justice system. (17) |
| One in 10 US Black men are put in solitary confinement before the age of 32. (12) |
| According to the United Nations, solitary confinement is defined as torture as it can lead to PTSD and suicide. Black men in the US are sent to solitary confinement for a longer period of time compared to their counterparts. (17) |
| People who are incarcerated with mental health illness of all races suffer mistreatment and medical neglect, and have high rates of suicide and self-harm. But people of color with mental health illness are even less likely to receive proper mental health services.(9) |
| Inmates of color are disproportionately punished and placed in solitary confinement, which has been shown to exacerbate mental illness. Many individuals experience their first psychotic episode in these conditions. (9) |
| Racial bias often prevents people of color from qualifying for diversion programs that could keep them out of jail and receiving mental health treatment in jail. (9) |
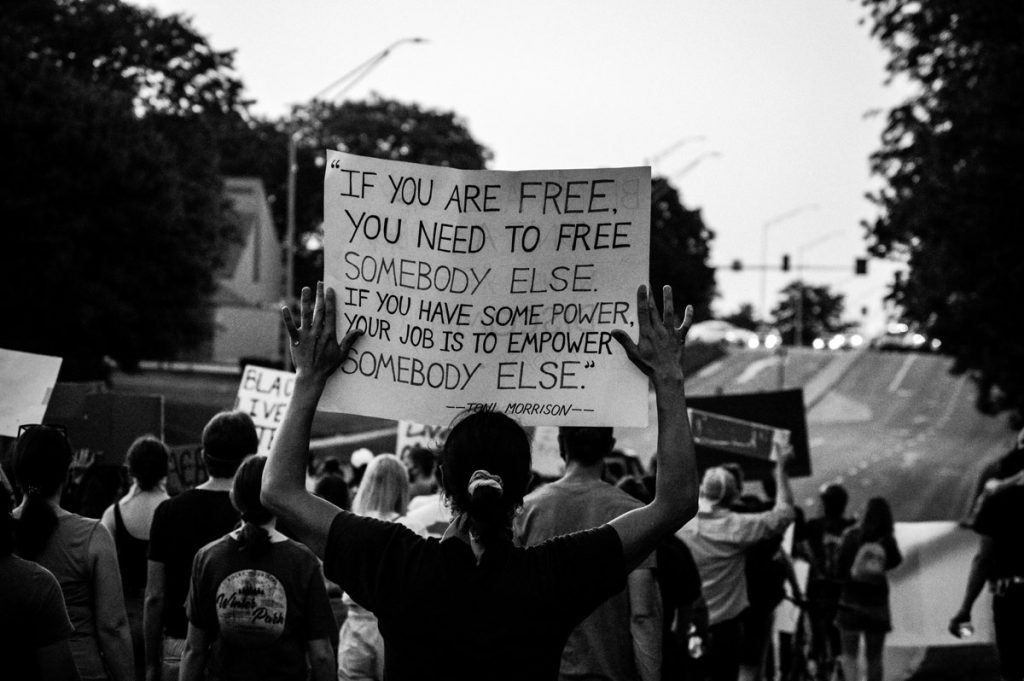
| Racism, Mistrust, and Barriers in Access to Care |
| Mistrust of medical and mental institutions is rooted deeply inside the Black community as a result of generations of racism, discrimination and trauma. (11) |
| As a result of racism, Black people are at an increased risk of developing psychosis, in part due to high amounts of chronic stress and trauma.(11) |
| Racial trauma can increase the risk of people of color meeting the criteria for Post-traumatic Stress Disorder. Stress plays a crucial role in how racism impacts both mental and physical health.(15) |
| Microaggessions are a form of racial trauma which can harm a person of color’s identity and sense of self-worth potentially impacting their mental health. (10) |
| Black children are more likely than White children to be put in a restraint during ED visits. According to research, systemic bias, racism, and “adultification” of Black youth, specifically Black boys, may impact the way they are perceived by nurses, doctors, and other specialists.(19) |
| Although Black families have more contact with mental health providers, fewer Black individuals seek out family psychoeducation and other essential aspects of the treatment process due to historic mistrust in the system. (11) |
| People from racial and ethnic minority groups are disproportionately affected by lack of access to quality health care, health insurance, and/or linguistically and culturally responsive health care. (20) |
| More than 80% of Black Americans are very concerned about the stigma associated with mental illness, which discourages them from seeking treatment. (21) |
| Lack of cultural understanding by health care providers may contribute to underdiagnosis and/or misdiagnosis of mental illness in people from racially/ethnically diverse populations. (7) |
| Language differences between patients and providers, stigma of mental illness in communities of color, and cultural presentation of symptoms can contribute to misdiagnoses. (7) |
| According to research from the Satcher Health Leadership Institute at Morehouse School of Medicine, racial mental health disparities cost the United States around $278 billion between 2016 and 2020 as a result of premature deaths that has been linked back to mental health, substance use disorder and suicide.(11) |
| Other BIPOC Health Facts |
| COVID-19 has disproportionately affected Black individuals in the U.S., and vaccination rates among Black individuals trail those of other racial groups. (18) |
| These results suggest that this might be less likely the result of vaccine hesitancy than other factors such as access, distant vaccine sites, lack of transportation and inflexible work hours. (18) |
| By December 2020, only 36% to 49% of Blacks and African Americans (compared with 44%-59% of White individuals) intended to be vaccinated when they became eligible. (18) |
| Non-Hispanic Black women are overrepresented in the number of deaths reported among women with confirmed COVID-19 regardless of pregnancy status, and Non-Hispanic Black pregnant women are at increased risk for developing severe COVID-19 symptoms compared with non-Hispanic White women. (8) |
| Black women are 3x more likely to die from a pregnancy-related cause than White women. (8) |
| Multiple factors contribute to these disparities, such as variation in quality healthcare, underlying chronic conditions, structural racism, and implicit bias. (8) |
| BIPOC are more at risk for complications from heart disease than white Americans. This includes a higher death rate and is partly due to the barriers to healthcare BIPOC groups face. (5) |